
Discoverers of insulin, Charles Best (1899 – 1978) and Frederick Banting (1891 – 1941) (right) on the roof of the medical building, Toronto University.
(Photo by Hulton Archive/Getty Images).
A Brief History of Insulin Discovery
The discovery of insulin has positively impacted the lives of Canadians and people around the world. Insulin has revolutionized the treatment of diabetes and paved the way for other medical advancements.
The discovery of insulin has positively impacted the lives of Canadians and people around the world. Insulin has revolutionized the treatment of diabetes and paved the way for other medical advancements.
In 1921, Canadian-born, Frederick Banting was a young surgeon whose interest in diabetes grew after reading medical papers about the pancreas. A loose scientific finding found that some sort of internal secretion of the pancreas was important in preventing diabetes and controlling normal metabolism. This research prompted Banting to note an idea for experimentation. Banting collaborated with a team at the University of Toronto (U of T), which included physiology professor J.J.R. Macleod, and biochemistry student Charles Best. The team worked tirelessly testing Banting’s theory and trying new experiments with pancreatic extracts. By the end of the year, the team was able to purify and refine the extract, and the first form of insulin was created.
In January 1922, Leonard Thompson, a 14-year-old boy dying from diabetes in Toronto, became the first person to receive an injection of insulin. The injection was successful and Thompson recovered and regained his strength. The discovery of insulin was a tremendous milestone that truly revolutionized both the therapy and prognosis of those with diabetes.
Frederick Banting and J.J.R. Macleod’s achievements were recognized internationally, and in 1923, they were awarded the Nobel Prize for Medicine.
Insulin Trivia!
Answer
“Insulin does not belong to me, it belongs to the world.”
-Frederick Banting
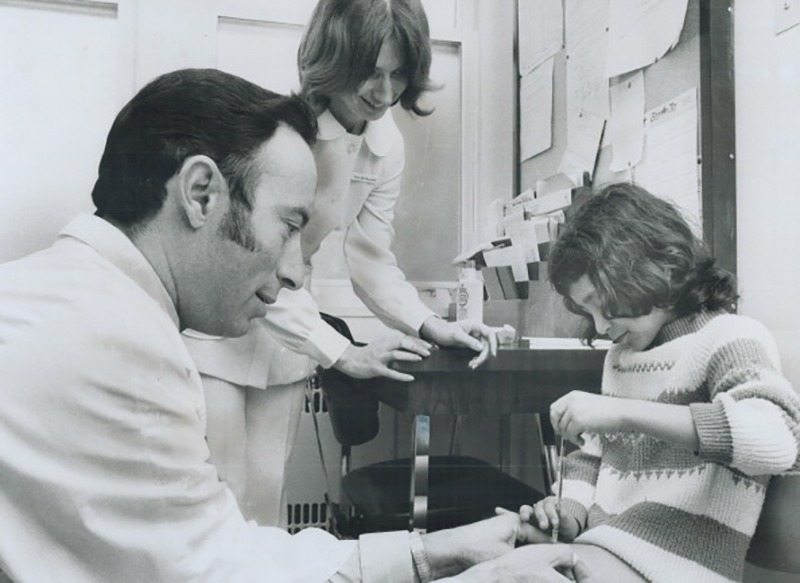
CANADA – APRIL 13: The Canadian Diabetes Association is raising funds to be used to teach diabetic children how to give themselves injections of life-saving insulin. Elma Couto; 10; already has the skill and demonstrates it for Dr. Robert Ehrlich and Nurse Ada McLeod; from Toronto’s Hospital for Sick Children. (Photo by Jeff Goode/Toronto Star via Getty Images)
Pharmacy’s Early Involvement with Insulin
Eli Lilly & Co. (now known as Lilly Canada) was the first pharmaceutical firm to offer assistance to U of T to develop the insulin extract.
Eli Lilly & Co. (now known as Lilly Canada) was the first pharmaceutical firm to offer assistance to U of T to develop the insulin extract.
U of T’s Connaught facilities spearheaded insulin production and developed a collaborative agreement with the pharmaceutical firm to protect the manufacturing and sale of what would eventually become the world’s first commercially available insulin. Later, they would collect licensing and royalties from other commercial firms that wished to produce insulin. These proceeds assisted in establishing a research fund at the University.
By November 1923, the Connaught facility was producing 250,000 units of insulin weekly. During this period the average person with diabetes needed 15–20 units every day. Dr. Charles Best and Dr. David A. Scott led the staff at Connaught and managed insulin production as it was now being exported from Toronto to locations and facilities across the globe. Locally, diabetes clinics were established at the Christie Street Veterans Hospital, Toronto General Hospital, and the Hospital for Sick Children.
Insulin Trivia!
Answer
The Transformation of Patient Care and Insulin Delivery
Medical advancements for diabetes management quickly followed insulin discovery and transformed patient care. In 1924, Becton, Dickinson and Company (BD) introduced the first dedicated syringe for insulin injection.
Medical advancements for diabetes management quickly followed insulin discovery and transformed patient care. In 1924, Becton, Dickinson and Company (BD) introduced the first dedicated syringe for insulin injection.
Prior to the creation of the dedicated syringe, people with diabetes would need to use large and heavy reusable syringes with plungers, barrels, and long large-bore needles. The process to sterilize the syringes and reusable needles was tedious as they would need to be boiled to ensure efficient reuse. The development of new and dedicated syringes improved insulin delivery, reduced pain, and the incidence of needle-associated infections.

Continuous research and advancements paved the way for other milestones in insulin delivery and diabetes management. Glucose monitoring tools initially began with simple urine sugar screening tests and the Clinistix® by Ames was the first dip-and-read test for glucose in urine. The evolution of meters permitted easier use and more variation in designs and technology. In 1981, Bayer Diabetes Care (now known as Ascensia Diabetes Care) created the Glucometer®, the first personal blood glucose meter that was portable and light-weight. Today’s blood glucose monitoring tools include advanced technologies that allow ease of use, tracking solutions, and quick accurate results.
The expansion of diabetes management therapies now includes ergonomic features that make injecting as painless as possible, additional user-friendliness, accuracy, and convenience. Patients with diabetes have greater flexibility to select insulin delivery and blood glucose monitoring tools that fit their individual needs and preferences.
Insulin Trivia!
Answer

The Evolving Role of Pharmacy Professionals in Diabetes Management
According to Diabetes Canada, there are close to 11 million Canadians living with diabetes or prediabetes, and the rates continue to rise.
According to Diabetes Canada, there are close to 11 million Canadians living with diabetes or prediabetes, and the rates continue to rise.
As one of the most easily accessible healthcare providers, pharmacy professionals are in a key position to assist with patients’ health, screening, and management of the disease. Diabetes treatments have made great advancements; today, there are various options to support the management of people with diabetes including medications, both oral and injectable, as well as continuous insulin pump therapy.
Pharmacy professionals are integral team members in providing patient care for individuals with diabetes. They assist patients with the fundamentals and intricacies regarding treatment implementation and management. With the increase in treatment options available, pharmacists also help guide patients with medication selection, administration, self-monitoring of blood glucose, and can also answer common questions and concerns.
Pharmacy professionals contribute to diabetes management in a variety of settings. In family health teams, pharmacists work within an interprofessional team to provide group or individual sessions on medication management, self-monitoring of blood glucose, nutrition, etc. for those with diabetes or pre-diabetes. In hospitals, pharmacists play a key role in discharge counselling, especially for individuals who may have been newly diagnosed with diabetes and have been prescribed insulin or oral medications and a glucometer. To help support the management of the disease, pharmacy professionals may collaborate with a patient’s diabetes care team to develop individualized plans for a patient’s blood glucose target. Pharmacy professionals are invested in helping patients manage the disease and support increased adherence to therapy.
Insulin Trivia!
Answer

Additional Resources
Thank You to Our Partners
©2021 Ascensia Diabetes Care Canada Inc.
For a full list of trademarks click here.


